Cancer immunotherapy: getting a little help from ourselves
Beginning with the approval of Rituximab in 1997, immunotherapies, therapeutics that use the body’s own immune system, have become popular in the fight against cancer. Because immune cells are innately capable of detecting abnormalities in a cell, researchers are developing strategies to harness this ability to destroy tumors with little to no side effects. But before many of these treatments ever see a human being, they are developed and tested for efficacy and safety in laboratory mice. Below, I review some of the strategies and mouse models that have been used to develop this exciting area of therapeutic research.
What is cancer immunotherapy?
Traditional cancer chemotherapy and radiation treatments are toxic and have many side effects because they indiscriminately kill both cancerous and normal cells. Immunotherapy is a promising approach to enhance specificity and reduce off-target effects. Cancer cells often express mutant or normal proteins at supra-physiological concentrations on their cell surfaces, which can be recognized by the host’s immune system. Through this mechanism, the immune system monitors protein synthesis inside cells and directs cytotoxic natural killer (NK) cells and CD8+ T cells to eliminate tumor cells that express proteins at the wrong time, concentration, or configuration. Additionally, B cells also play a role in this process by coating the cell expressing aberrant proteins with antibodies. Subsequently, other immune cells, including macrophages and NK cells, as well as complement, become activated, triggering antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC), respectively, to destroy the tumor cell.
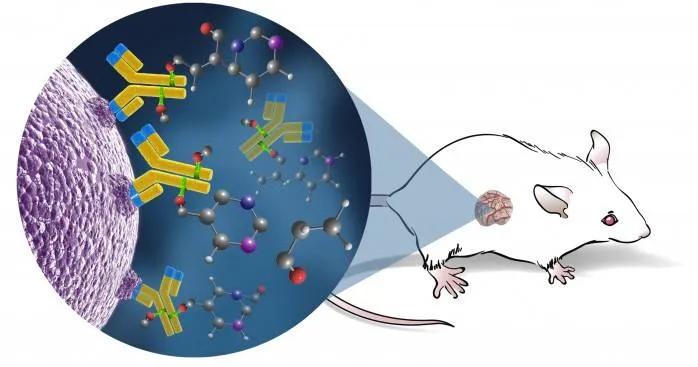
Researchers have pursued several immunity-based strategies to combat cancer, including creating synthetic antibodies that target tumor cell antigens, developing cell-based therapies that enhance T and NK cell anti-tumor responses, and employing cytokine therapies that activate immune cells to target the tumor. These treatments act by initiating apoptosis, delivering chemotherapeutic drugs (known as antibody-drug conjugates), inhibiting growth factor signaling, enhancing tumor cell recognition by host immune cells, or initiating ADCC or CDC. For example, Rituximab, the first cancer immunotherapy approved for treating leukemia and lymphoma, is an anti-CD20 monoclonal antibody that induces apoptosis in malignant B cells and initiates ADCC and CDC by the patient’s own immune system. Keytruda, another monoclonal antibody targeting the PD-1 receptor (a protein overexpressed in several cancers that can inhibit T cell proliferation) was initially approved in September 2014 for treating metastatic melanoma, subsequently in March 2022 for endometrial carcinoma, and most recently in December 2023 for the combination treatment of metastatic bladder cancer.
With the promising potential of immunotherapies and numerous cancer immunotherapies in development, the necessity for preclinical in vivo models facilitating reliable, valid, and rigorous testing of these therapies is paramount to efficient translation in clinical studies. JAX has been leading the charge, pioneering the creation and validation of humanized mouse platforms. These platforms not only harbor human-specific drug targets but also express these targets within an environment that closely mirrors human immune biology. Such models provide the framework for conducting clinically predictive PK/PD, efficacy, and safety testing of immunotherapies.
Which mouse models can be used for developing cancer immunotherapeutics?
Historically, immune-competent mouse models such as BALB/cJ, DBA/2J, and C57BL/6J mice have been used to evaluate cancer vaccine efficacy and to evaluate ADCC and CDC responses to immunotherapy delivery (for examples, see Humar et al., Liu et al., and Ramakrishnan et al.). These inbred strains serve as excellent initial investigation platforms to measure a therapy’s efficacy against mouse tumors and cell lines.
Counterintuitively, immunodeficient mouse models are the superior platform in the preclinical drug pipeline for predicting the behavior of immunotherapy candidates in the clinic. Unlike immune-competent models, these immunodeficient models support the engraftment of both human tumors and human immune cells, thereby allowing for a more comprehensive recapitulation of human pathophysiology. This capability enables reliable early assessment and refinement of lead molecules to minimize toxicity and increase efficacy prior to human trials.
Immunocompromised strains such as inbred nude mice, NOD scid, NRG, and NSG have all been used to develop new immunotherapies using primary human cancer xenografts. For example, in a study using 48 patient-derived colorectal cancer xenograft models in nude mice, a comparative analysis of two antibody-drug conjugates was performed to determine efficacy in inhibiting tumor growth. In another study, NOD scid mice injected with primary AML cells were used to demonstrate efficacy of an antibody-drug conjugate in reducing tumor load. Finally, inNSG mice injected with primary AML cells, a single dose of an anti-CD33 ADC was effective in inhibiting tumor growth. None of these studies could have been performed in an immunocompetent strain.
What advantage does the NSG mouse have over other immunodeficient models?
Immunodeficient models, while valuable for investigating cancer cell mechanisms, vary in their suitability for different types of studies. Nude mice [(NU/J (002019), B6-nude (000819), J:NU (007850)] are well suited for hosting established, rapidly growing tumor cell lines. However, because nude mice still have B cells and robust NK cell responses, they are not suitable hosts for blood-borne cancers, slow-growing human or mouse primary tumor cells, or heterogenous tumor fragments. Additionally, both inbred and outbred nude mice are inadequate hosts for engrafting human immune cells.
In contrast, NSG and NRG mice, being severely immunodeficient (T and B-cell deficient), are excellent hosts for engrafting slow-growing primary cell lines, patient-derived xenografts, blood-borne cancers, and human immune cells. They serve as the optimal “base model,” supporting the engraftment or co-engraftment of human tumors and human immune cells. By engrafting these mice, researchers can simulate conditions closely resembling those observed in human patients. Of note, the primary difference between NSG and NRG is that NRG mice are more resistant to irradiation and genotoxic drugs, making them the optimal choice for studies requiring a radioresistant host.
One of the most exciting models to test novel immunotherapies is the combination of mice hosting both the human immune system and patient-derived tumors.
Where can I get humanized NSG mice?
If you’re interested in humanized NSG mice, you’re in luck! We have readily available hu-CD34 and hu-PBMC engrafted mice. Furthermore, we are continually developing new NSG variants that support different ratios of specific human immune cell populations. Check out our immune-humanized webinar to learn more. And if you are interested in using or learning more about NSG mice, don’t forget to check out the NSG resources page. Here, you can find useful information about housing these mice at your facility, FAQs, related NSG-based strains, and breakthrough research using NSG mice.
Want to learn more about our PDX models for cancer research?
Please visit the PDX Resource at the Mouse Tumor Biology database to see our current offerings and characterization studies for many of these models. And if you’re looking to save some time and money, check out our PDX Live program where many of our most popular PDX models are engrafted and ready to be put on study.
