All eyes on Alzheimers disease research
The Search Magazine Article | April 8, 2019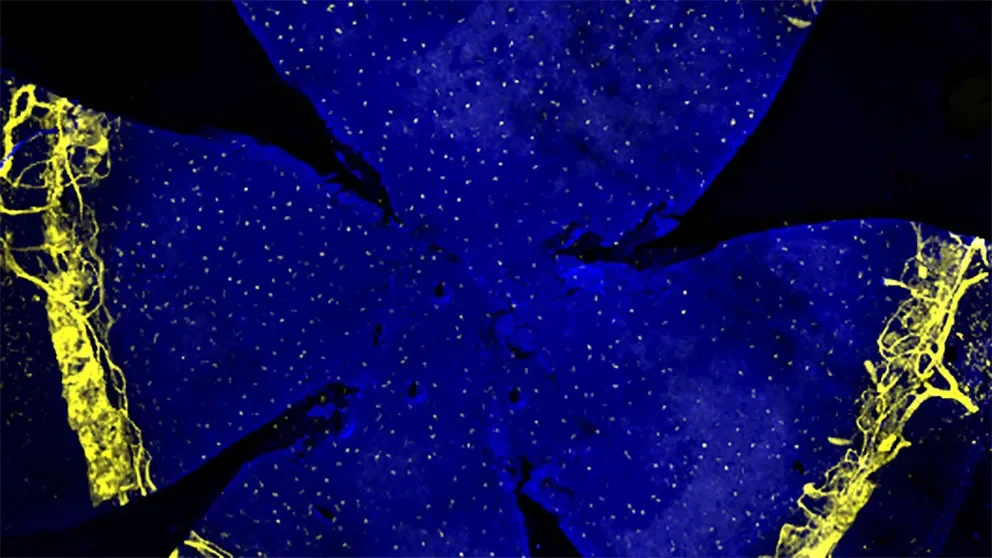
The retina’s interaction with the brain makes it a good and relatively accessible platform for studying neural development.
Gareth Howell is a JAX associate professor who studies Alzheimer’s disease. His research has shown that there are several connections between Alzheimer's disease and glaucoma.
In glaucoma, the clear fluid that flows continuously through the anterior chamber at the front of the eye doesn’t drain properly, leading to a buildup of pressure that can damage the optic nerve, leading to vision loss and blindness. An estimated 60 million people worldwide, and 3 million Americans, have glaucoma, and according to the World Health Organization it is the second leading cause of blindness (after cataracts).
We are looking at the eye as a window to the brain for diseases like Alzheimer's disease.
Just as a skin infection causes immune cells to rally to the site to mount an inflammatory response to fight it off, nerve cells have their own army of protective immune-like cells, including microglia, and immune cells such as monocytes and macrophages found in the optic nerve head or the brain.
“These immune-like support cells help to clear amyloid plaques in the brain in Alzheimer’s disease and respond to high intraocular pressure in the case of glaucoma,” Howell explains. Harnessing the immune-like response could point to new treatment strategies for both diseases.
Howell and his lab have also identified a protein called MEOX2, which appears to have a role in plaque deposition in Alzheimer's disease. “Our gene profiling studies predicted it also played a role in glaucoma,” he says. Howell's research team looked to the DBA/2J mouse, which develops glaucoma as humans do, in middle age (8-13 months for a mouse). “If you reduce protein levels of MEOX2, glaucoma is worse,” Howell says. “We want to know if there are ways to control MEOX2, or its downstream targets, to switch the environment from a damaging one to a beneficial one.”
“In addition,” Howell says, “we are looking at the eye as a window to the brain for diseases like Alzheimer's disease. We’re particularly interested in blood vessel health in the brain. We hypothesize that in Alzheimer's retinal vessels may decline in a similar fashion to brain vessels. If proven, it would allow us to use retinal vessel health as a proxy for brain vessel health to identify those at risk of Alzheimer's disease before dementia-like symptoms develop.”

