Induction of autoimmunity in humanized NSG mice
The highly immunodeficient NSG mice (005557) are the current state-of-the art host for engrafting human hematopoietic stem cells (HSC) and establishing human immunity in a small laboratory animal. A new publication in the Journal of Immunology (Vudattu, N. et al. 2014) provides evidence that treatment of these “humanized” mice with ipilimumab (CTLA-4 Ig) can disrupt immune tolerance and initiate features of autoimmune disease in mice. This research establishes humanized NSG mice as a therapeutic platform to study human specific pathogenesis of autoimmunity and develop new therapeutic interventions with greater potential to translate to human patients suffering from a wide range of autoimmune diseases such as type 1 diabetes, lupus and multiple sclerosis.
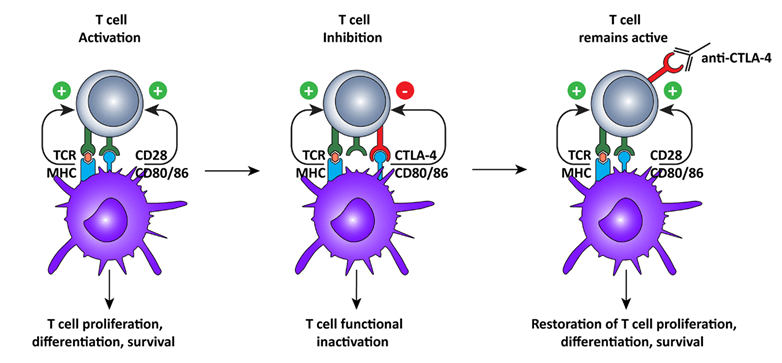
Figure 1. Cytotoxic T lymphocyte-associated antigen-4 blockade restores T cell activation.
After recognition of MHC:peptide complex by the TCR, the second signal for T cell activation is provided by binding of CD80 or 86 to CD28 on the T cells. This interaction leads to cell surface expression of CTLA-4, which has a higher affinity for CD80/86, thus interrupting the activation signal. Additionally, the signal delivered via CTLA-4 down-regulates T cell function and inhibits excessive expansion of activated T cells. Anti-CTLA-4 monoclonal antibodies bind to CTLA-4, and block the interaction with CD28, which is again free to interact with CD80/86, prolonging T cell activation and amplifying T cell-mediated immunity against tumors. Image from: Vasaturo, A., et al. (2013). "Clinical Implications of Co-Inhibitory Molecule Expression in the Tumor Microenvironment for DC Vaccination: A Game of Stop and Go." Front Immunol 4: 417. PMID: 24348481
Regulation of T cell responses by CTLA-4
Activation of T cells requires a complex interaction between cell surface molecules on the T cell and the antigen presenting cell. Engagement of the T cell receptor with peptide bound in an antigen-presenting protein alone is not enough to stimulate T cell proliferation, cytokine production and effector function. There are a number of co-stimulatory molecules that play an important role in the regulation of T cell activation, anergy and immune tolerance.
Proteins on the T cell that play a key role in co-stimulation are CD28 and cytotoxic T lymphocyte-associated molecule-4 (CTLA-4). These proteins engage B7 molecules (CD80 and CD86) on the antigen-presenting cell. When CD28 engages B7 molecules during T cell receptor binding, the T cell becomes activated. CTLA-4 is highly homologous to CD28 and can also bind the B7 molecules, playing a complex role in regulating T cell function. High expression of CTLA-4 is thought to compete with CD28 and, when bound to B7, can suppress activation of T cells.
Regulatory T cells (Treg), which are important in maintaining immune tolerance, constitutively express CTLA-4. When CTLA-4 expression is low, CD28 is bound and the T cell is activated. However, mice with a null mutation in CTLA-4 develop an autoimmune lymphoproliferative disorder. Blockade of co-stimulation has been demonstrated using a fusion protein composed of CTLA and IgG1 (CTLA-4 Ig), also known as ipilmumab. Ipilmumab is an approved treatment for patients with metastatic melanoma. Treatment increases the effector to Treg ratio and leads to enhanced killing of tumors. Unfortunately, many patients treated with ipilmumab also developed a number of features of autoimmune disease.
Creation of a mouse model of human autoimmune disease
There are a number of strains of mice that develop autoimmune disease with significant similarity to their human counterpart. However, there are a number of distinct differences between human and mouse immune function. These differences are thought to explain why many preclinical therapeutic interventions in autoimmune mice fail to translate to human clinical applications. Recognizing this, Vudattu et al. chose to develop a mouse with human autoimmune disease.
The small laboratory animal capable of supporting human HSC engraftment and establishment of human immune function is the NSG mouse (NOD scid gamma, or NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ). These researchers treated humanized NSG mice with CLTA-4 Ig to induce autoimmunity. Following treatment, 80% of the mice lost nearly 15% of their body weight by 30 days. The animals showed lymphoploliferation as indicated by enlarged spleens as well as mesenteric and peripheral lymph nodes. Liver, adrenal cortex and salivary glands contained infiltrates consisting of CD4+ and CD8+ T cells, B cells and macrophages. Liver damage was indicated by increased alanine aminotransferase (ALT) activity and decreased serum albumin level. The mice were also positive for human autonuclear antibodies (ANA). These immune responses were not considered a graft-versus-host disease (GvHD) because the mice did not have dermatitis or diarrhea, and lacked lymphocytic infiltrates in the skin, oral mucosa and colon. Finally, symptoms of autoimmune disease were decreased or eliminated by treatment with the T cell-depleting antibody, treplizumab (anti-CD3 mAb).
The research presented by these authors provides evidence that humanized NSG mice can be induced to develop autoimmune disease, establishing these mice as the first small-animal model of human specific autoimmunity. Researchers and clinicians now have a new important tool to study the pathobiology of human autoimmune disease. This platform should enable the development of new therapeutic interventions with greater potential for translation to the clinic.