JAX® Mice aid plague vaccine development
October 4, 2010From the first recorded pandemic of the plague in the Byzantine Empire in the sixth century through the last major outbreak in Vienna in 1679, the "Black Death" is thought to have killed approximately 200 million people. Thanks to a better understanding of the disease, outbreaks are uncommon today – even though the bacteria that cause it are still present in rodent populations worldwide. Although several antibiotics can treat the plague, some antibiotic-resistant strains have evolved. Concern that the plague may be used as a biological weapon by terrorist organizations is intensifying efforts to develop a safe and effective vaccine. With the help of several JAX® Mice strains, a research group led by scientists at the Trudeau Institute, Saranac Lake, NY, has made important contributions to that end (Kummer et al. 2008; Szaba et al. 2009; Lin et al. 2010).
The plague
Plague is caused by Yersinia pestis (Y. pestis), a Gram-negative bacterium transmitted naturally among infected mammals, most commonly rats, via flea bites. Initially, it manifests itself in the "bubonic" form, characterized by "buboes" – swollen lymph nodes in the armpits and groin. Sometimes buboes do not develop, in which case the plague is termed septicemic. In either case, the infection causes fever, headache, malaise and gastrointestinal problems. If detected early, before symptoms develop, plague can be treated; if left untreated, it can progress to the lung and develop into secondary pneumonic plague. The plague can also be transmitted from an infected person or other animal through the air, in which case it develops into primary pneumonic plague, the most feared and virulent form of the disease, and the form bioterrorists would likely use. Pneumonic plague is particularly feared because infection can go undetected until symptoms develop (Alpar et al. 2001;CDC).
Plague vaccine approaches
Several plague vaccines have been developed, but none are completely safe or effective against all forms of the disease. Due to ethical concerns over purposefully exposing humans toY. pestis, human clinical trials can only address vaccine safety. To determine vaccine efficacy and clinically relevant immune responses, researchers must rely on animal models.
Killed whole cell Y. pestis vaccines
Some plague vaccines were developed with killed whole cell preparations ofY. pestis. In mouse models, such vaccines confer moderate protection against bubonic plague but relatively little against pneumonic plague (Hill et al. 2003). As many as 25% of people vaccinated experience side effects, which may be quite severe. Consequently, whole-cell vaccines are no longer used in the United States.
Subunit vaccines
Vaccines comprised of subunits of the F1 and/or LcrV proteins found on the cell walls ofY. pestis are effective against pneumonic plague in animal models, including some non-human primate species. However, the antibodies generated by such vaccines may not be good indicators of how protective the vaccines are. Evidence from the Trudeau team (Kummer et al. 2008; Szaba et al. 2009; Lin et al. 2010) and other investigators indicates that, to be sufficiently effective against all forms of the plague, a vaccine must marshal not only the body's antibody (B cell-mediated) immune defenses but also its cellular/cytokine (T cell-mediated) defenses. For example, in 2008, the Trudeau team reported that not only do cytokines TNFAand IFNG play a significant role in mediating an F1/LcrV vaccine's passive protection to C57BL/6J (000664) mice from an intranasal infection with a partially weakened Y. pestis strain, but they confer antibody-independent protection against the virus in similarly infected B cell-deficient B6.129S2-Igh-6tm1Cgn/J (002288) mice (Kummer et al. 2008). In a more recent study, the team demonstrated that the two cytokines also play a significant role in mediating both passive and active immunity conferred to C57BL/6J mice by an F1/LcrV vaccine against an intranasal infection by a fully virulentY. pestis strain (Lin et al. 2010). These studies were followed by clinical trials to test the efficacy and safety of F1/LcrV vaccines in humans.
Live but attenuated Y. pestis cell vaccine is safe and effective in mice
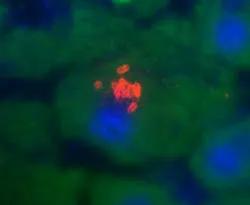
C57BL/6J mice were used to demonstrate that TNFA and IFNG play an antibody-independent role in mediating vaccine protection against the plague.
Vaccines comprised of living (but weakened) organisms generally marshal both B cell-mediated and T cell-mediated defenses. Such a plague vaccine was developed in Europe over a century ago and administered to millions of people. However, it has not been proven safe and effective against all forms of the plague in animal models. Neither this nor other such vaccines have ever been licensed in the United States.
In 2009, the Trudeau team reported developing such a vaccine that is effective in mice. The vaccine contains an entirely avirulent strain ofY. pestis and completely protects C57BL/6J mice against an intranasal challenge with a partially virulent Y. pestis (Szaba et al. 2009). Additionally, using T cell-deficient B6.129P2-Tcrbtm1MomTcrdtm1Mom/J (002122), and B cell-deficient mouse strains, the team demonstrated that T cells confer most of the protection: the vaccine is effective in B cell-deficient mice unless they are depleted of CD4 and CD8 T cells. If TNFA and IFNG are neutralized at the time of infection, the vaccine is ineffective. Although the vaccine does not prevent bacteria from being disseminated from the lungs, it limits their growth and pathology. The Trudeau team's results suggested that a similar vaccine would effectively protect humans against pneumonic plague.
References
Alpar HO, Eyles JE, Williamson ED, Somavarapu S. 2001. Intranasal vaccination against plague, tetanus and diphtheria.Adv Drug Deliv Rev 51:173-201.
Kummer LW, Szaba FM, Parent MA, Adamovicz JJ, Hill J, Johnson LL, Smiley ST. 2008. Antibodies and cytokines independently protect against pneumonic plague.Vaccine 26:6901-7.
Hill J, Copse C, Leary S, Stagg AJ, Williamson ED, Titball RW. 2003. Synergistic protection of mice against plague with monoclonal antibodies specific for F1 and V antigens ofYersinia pestis. Infect Immun 71:2234-8.
Kummer LW, Szaba FM, Parent MA, Adamovicz JJ, Hill J, Johnson LL, Smiley ST. 2008. Antibodies and cytokines independently protect against pneumonic plague.Vaccine 26:6901-7.
Lin JS, Park S, Adamovicz JJ, Hill J, Bliska JB, Cote CK, Perlin DS, Amemiya K, Smileya ST. 2010. TNFA and IFNG contribute to F1/LcrV-targeted immune defense in mouse models of fully virulent pneumonic plague.Vaccine. 2010 Sep 11. [Epub ahead of print].
Szaba FM, Kummer LW, Wilhelm LB, Lin JS, Parent MA, Montminy-Paquette SW, Lien E, Johnson LL, Smiley ST. 2009. D27-pLpxL, an avirulent strain ofYersinia pestis, primes T cells that protect against pneumonic plague. Infect Immun 10:4295-304.
