Novel antibody tests reveal complexity of the immune response to SARS-CoV-2
Research Highlight | July 28, 2020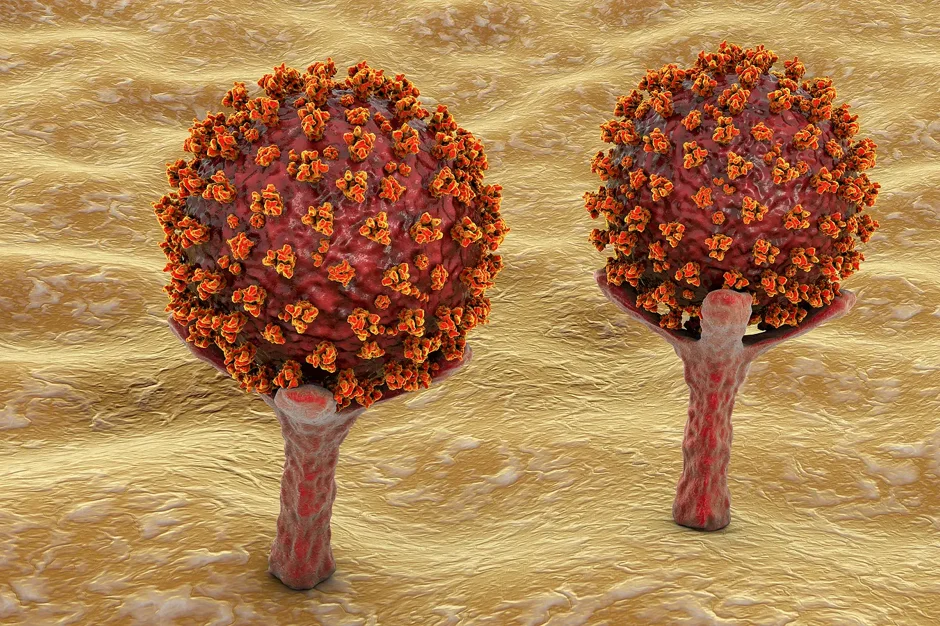
The interaction of SARS-CoV-2, the novel coronavirus causing the global COVID-19 pandemic, and the human immune system is the focus of intensive research. The ability of antibodies to target SARS-CoV-2, particularly the spike protein essential for viral entry into cells, may help determine disease susceptibility and progression in patients.
Leveraging expertise developed from his extensive work with HIV, Jackson Laboratory (JAX) Professor Derya Unutmaz, M.D., led an effort to develop an assay that determines how well anti-SARS-CoV-2 antibodies are able to neutralize binding with ACE-2, the human receptor for the virus. Using a non-infectious pseudo-virus with the SARS-CoV-2 spike protein on the external membrane, the assay does not require a BSL-3-level biosecurity facility, yet detects the presence of neutralizing antibodies with extremely high sensitivity and specificity. In a pre-print posted on medRxiv, Unutmaz shows that the assay is able to detect neutralizing antibody in patient plasma even at high dilutions, up to a million-fold.
Working with samples from 87 total subjects, from three different centers (SUNY Downstate Medical Center, UConn School of Medicine and Cedars-Sinai Medical Center) as well as healthy controls (from year-old frozen samples to ensure non-infection), Unutmaz and his team were able to determine accurate antibody levels in every patient. The assay is also sufficiently sensitive to distinguish background levels of antibody in control samples which may have been from anti-SARS-CoV-2 antibodies in patient plasma. In addition, the assay provides the ability to identify antibody isotopes and assess the ratio of IgA, IgG and IgM present in each sample.
While work is ongoing to increase the number of patient samples analyzed, the preliminary findings already obtained with the assay are intriguing and indicate new areas to investigate further. First, samples from patients with severe disease—in the ICU or deceased—had almost 100-fold higher neutralizing antibody levels than those with cases mild enough not to require hospitalization. Why, then, did they get so sick? Could extremely high levels of antibody even be harmful? And how would that influence the use of convalescent plasma as a therapy in severely ill patients who already have high antibody levels?
Also, high IgG levels drive the increase in total neutralizing antibody in severe patients, while IgA levels are often lower in severe or fatal disease versus milder cases. More inquiry is needed, but given that IgA is secreted in mucosal tissues and is involved in front-line protection, it’s possible that IgA is more important for mitigating severe disease, and an IgG-initiated macrophage response is a component of more severe pathology.

