Immune system 2.0: Can we re-engineer the human immune response?
Research Highlight | July 30, 2018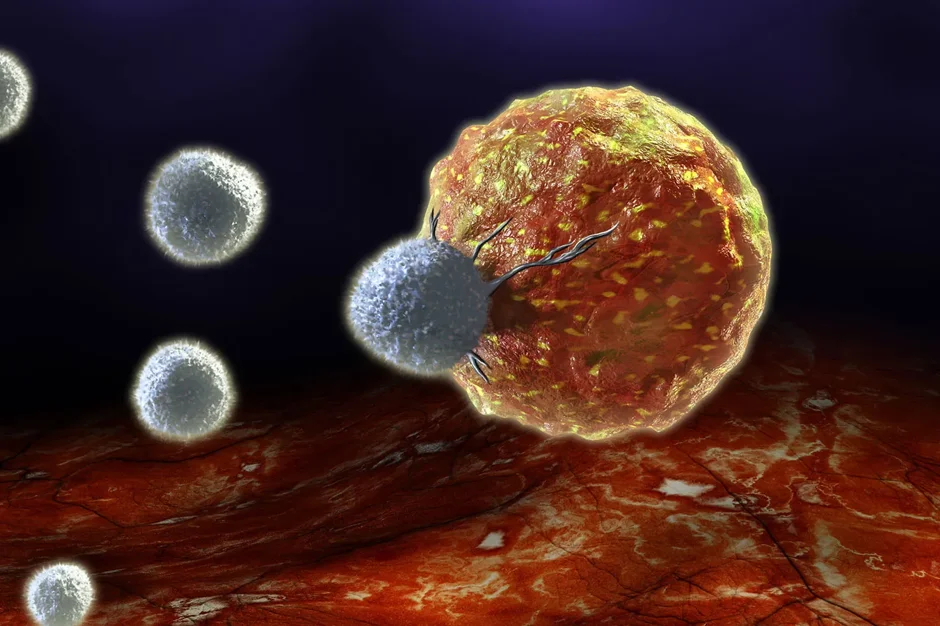
Genetic editing has progressed rapidly over the past several years, in large part because of the development and refinement of CRISPR/Cas9 technologies. Put simply, CRISPR/Cas9 allows accurate targeting of and changes to genetic sequences within cells, and it is relatively quick and easy to implement. Its potential applications are vast, and recently a team led by JAX Professor Derya Unutmaz, M.D., evaluated its use in immune cells. In “Functional Interrogation of Primary Human T Cells via CRISPR Genetic Editing,” published in the Journal of Immunology, the researchers demonstrate the ability to target and disrupt specific genes and/or alter their expression levels, which has important implications for both immunology research and clinical treatments.
Unutmaz and his team worked with primary human T cells. Subsets of T cells serve to regulate the immune response while others respond to infectious and other threats in a complex system of signaling and activation/suppression. Therefore, being able to tweak the response to counteract problems — such as decrease it in autoimmune disease or increase it to help fight cancer cells—would be of enormous medical benefit. The team used a lentiviral system to introduce CRISPR/Cas9 into the cells, leading to long-lasting, stable function of the editing system. They simultaneously deleted multiple genes in several types of T cells through normal Cas9 function. They also used a deficient version of Cas9 (dCas9, which doesn’t cut DNA but binds to it instead) to change promoter sequence function, leading to increased or decreased expression of specific genes.
So what might this mean? One of the genes knocked out, CD95, promotes cell death, which can be important when an immune response needs to be regulated down. But deleting it makes T cells more resilient and could enhance anti-cancer immune responses. Also, patients with mutations that disable a protein known as ORAI1 lack a process, Ca2+ influx, crucial for T cell function, and suffer from severe immunodeficiencies. Deleting it in T cells in culture provides a valuable way to analyze the molecular mechanisms underlying the human disease and similar studies can be performed with other immunodeficiency diseases with known genetic components. Finally, Unutmaz and his team were able to induce expression of a gene called GARP, using CRISPR tools, that mediates suppressive functions such as preventing autoimmunity or transplant rejection. In a similar strategy they increased expression of proteins known as CD25 and CD127, which enhanced interleukin signaling and could be used to induce a more effective T cell response in cancer patients.
While the study showcases the feasibility of the methods in a research setting, the results provide a tantalizing glimpse of what might be possible clinically. As the authors conclude: “A wide range of adaptations and applications of CRISPR-mediated genome engineering in human T cells also holds great promise for cell-based therapies for cancer, microbial infections, immune deficiencies, and autoimmune and chronic inflammatory disease."

