We change as we age.
On the surface, that’s a completely obvious statement. But most of the actual mechanisms of biological aging are invisible, occurring underneath our increasingly wrinkled skin. And many of those hidden processes, which change functions over time at a molecular level, remain poorly understood.
What happens to our bodies between ages 25 and 45, between 65 and 85, and every decade along the way? Why do we become ever more susceptible to various diseases over time? And do we all age in the same way, or are there differences?
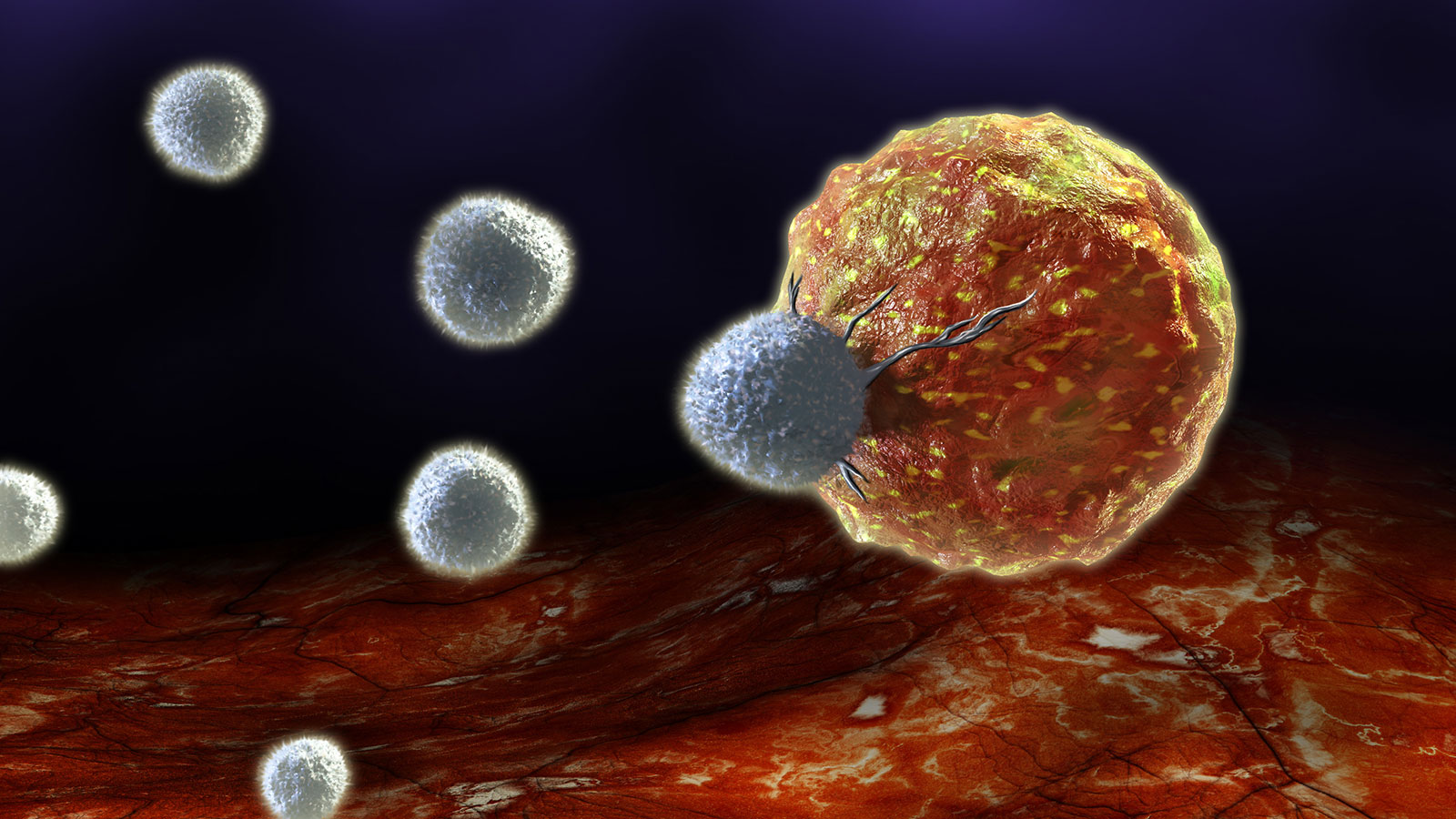
Weakening immune response
A vital element of the aging process involves our immune responses. Decades of observational clinical data have shown that immune systems grow weaker and more prone to dysfunction as we age. What serves as an effective protective mechanism in our youth becomes far less reliable, and it can even cause active harm. The elderly are therefore more prone to infections and inflammation and less responsive to vaccines than their younger peers. Researchers have also observed that immune responses differ between men and women, and that those differences can become more important with age. For example, on average women are more susceptible to autoimmune diseases, while men are more prone to infectious diseases. The exact reasons why have remained elusive, but advances in research capabilities allow scientists to probe exactly what happens within us as the years pass.
And while all the differences are clinically meaningful, the recent COVID-19 pandemic has increased both the awareness and urgency around understanding them in more detail. It quickly became apparent that the incidence of severe disease and death increased markedly with age, with anyone over 70 being particularly vulnerable regardless of their prior health status. Men and women also had significant differences in their responses to infection. While the pandemic crisis will hopefully ease, it has shown, in stark terms, how essential it is to study our immune mechanisms and improve our ability to address vulnerabilities.

Duygu Ucar.
Studying molecules gone awry
How can one determine age-related immune differences? The ideal situation would be to follow people over a long period of time, taking the sample specific samples at regular intervals. But these so-called studies, take decades to provide usable aging data. Instead, researchers at The Jackson Laboratory and UConn Health have teamed up to match healthy people as best they can between different age groups. Their early findings show that men and women experience immune changes with age, as expected, but both the changes themselves and the timing of the changes differ.
The study co-leaders, JAX Professor Jacques Banchereau, Ph.D., and Associate Professor Duygu Ucar, Ph.D.Develops computational models using genome datasets to study gene regulation and identify hypotheses for genomic medicine.Duygu Ucar, Ph.D., approach the work with very different perspectives and areas of expertise.
Banchereau is an immunologist who has extensive experience studying the molecular pathways involved with immune function. His research covers many facets of the field, including how the immune system mounts a defense against infectious pathogens, how it can be activated for cancer immunotherapy, and how vaccines can be developed to activate the best possible protective immune response. Banchereau is particularly interested in figuring out how to improve vaccine effectiveness in the elderly, who can be vulnerable to both familiar pathogens, such as influenza, and emergent pandemics.
Ucar is a computational biologist who specializes in assessing the state of the genetic material within cells and how it can affect particular genes’ activity. These molecular traits reveal essential characteristics of specific cells and identify functional differences between them. Ucar can detect even subtle changes with age between the same kinds of immune cells.
Human immune aging
Banchereau and Ucar’s research has revealed some intriguing insights into what happens to immune function as we age, and why changes occur. It has shown that many aspects of immune activity make a transition from mostly helping us to sometimes hurting us, especially once we reach certain ages. For example, a preliminary study looked at which genetic regions are more active in immune cells from young people than those from their older counterparts. It found changes in gene activity associated with adaptive immune function, the part of the immune system that responds to new situations, such as a new infectious microbes, and “remembers” the microbes to protect against them in the future. Not surprisingly, adaptive immunity-related genes are more active in younger people than in the elderly.
On the other hand, genes involved with innate immune activity (which provides initial, non-specific immune responses) and inflammatory processes are increasingly active with age. Inflammation involves chronic low-level immune activity even in the absence of pathogens, associated with autoimmune disease or obesity. And chronic inflammation has been linked to many diseases, including cancer.
Subsequent work has further revealed the specific ages at which significant molecular changes affect our immune function. The first was detected in the late 30s and early 40s, and the timing was similar in both sexes. The second, however, differed in both timing and magnitude between men and women, taking place in men between ages 62 and 64 and women, less profoundly, between ages 66 and 71. Interestingly, adaptive immune activity can increase in women over 65, giving them an advantage over men in fighting infections and providing a possible explanation for the increased incidence of autoimmune disorders. Men see increased activity associated with innate immune cells, which are less effective against pathogens and can be associated with inflammation.
The results are significant enough to have implications for clinical care. Men and women often need different therapies for them to be maximally effective. A better understanding of the changes can also help researchers explore ways that we might be able to target certain immune functions for enhancement or suppression. This would allow us to retain immune function like that of our youth.